Atefeh Galehdarifard, Mojgan Khademi, Mohammad Gholami, Moloud Radfar, Farzad Ebrahimzadeh and Mohammad-Hasan Imani-Nasab
This blog post is based on the Evidence & Policy article, ‘The impact of knowledge brokering on nurses’ empathy with patients receiving cardiac care: an experimental study’.
Empathy is a fundamental concept in the development of human relationships. Whether individuals have a natural inclination toward empathy or have cultivated it through education and upbringing, this background can significantly influence the effectiveness of interventions designed to promote empathetic behaviour. Our research suggests that individuals with higher levels of empathy are often more motivated to enact change, actively promote empathy, and show a greater willingness to learn and adopt empathetic behaviours in practice.
The importance of empathy in patients with cardiovascular diseases
Research by Dambha-Miller et al. (2019) has revealed that better empathy is linked to a lower risk of cardiac events (Dambha-Miller et al., 2019) , highlighting the need for cardiac nurses to engage in empathetic interactions with their patients. However, many nurses report facing significant challenges in establishing these connections, especially early in their careers (Dikmen et al., 2022).
Moreover, evidence shows a concerning lack of empathy among healthcare workers, particularly nurses (Hassankhani et al., 2022, Winter et al., 2022). Indicators such as indifference, neglect (Levett-Jones et al., 2017), and even violence detract from the compassionate care that patients deserve (Levett-Jones et al., 2019). When poor empathetic practices occur, they can distort the nurse-patient relationship, reduce the quality of care (Khademi et al., 2019), and ultimately lead to adverse health outcomes (Strekalova et al., 2017).
Addressing the research-practice gap
This situation underscores a significant research-practice gap in nursing empathy. To bridge this gap, we turned to knowledge brokering, a strategy designed to facilitate the translation of knowledge into practice (Nilsen, 2015). Our experimental study, involving 100 cardiac nurses, aimed to assess the impact of knowledge brokering on enhancing nurses’ empathy toward patients receiving cardiac care.
Findings
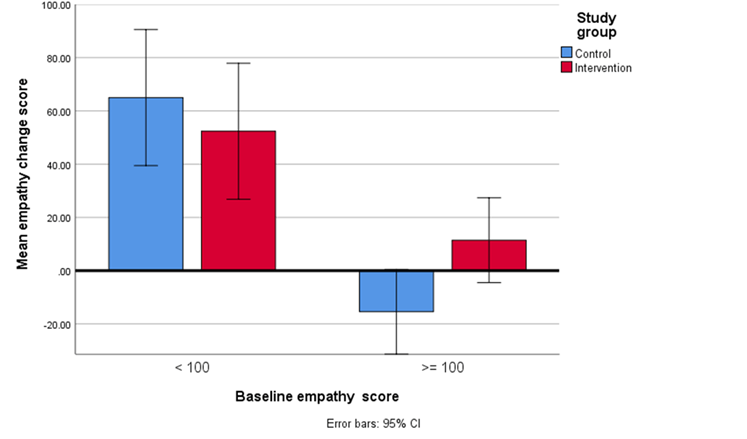
We recently published our study in Evidence & Policy, and here’s what we found: In the intervention group, which received special support, the Mean Empathy Change Score (MECS) improved significantly (p = .003). This indicates that knowledge brokering effectively enhances empathy among nurses. To better understand the differences in MECS between the groups, we analyzed the data based on their Baseline Empathy Score (BES) measured at the start of the study. We divided the participants into two categories: those with a BES under 100 (BES <100) and those with a BES of 100 or more (BES ≥100). For nurses with a BES of 100 or more – classified as moderately empathic – the MECS in the intervention group showed substantial improvement compared to the control group. This demonstrates that the knowledge brokering strategy was effective for these nurses. However, for nurses with a BES under 100, the MECS in the intervention group was lower than in the control group. This suggests that knowledge brokering was less effective for these individuals, indicating a need for additional support, attention, incentives, and training to foster their empathy (see Figure 1).
Conclusion
Our research shows that a knowledge brokering strategy is an effective way to boost empathy in nurses who already have a moderate level of empathy. The success of this approach depends on the nurses’ BES. We found that teaching empathy works best for those who already possess some level of it, whether it’s natural or learned through education. Because of this, we suggest including programs aimed at enhancing empathy in the education of young children. By doing so, we can help raise more empathetic individuals who will positively impact society, especially in healthcare. In short, investing in empathy education today can lead to a kinder, more compassionate future for everyone.
References
DAMBHA-MILLER, H., FELDMAN, A. L., KINMONTH, A. L. & GRIFFIN, S. J. 2019. Association between primary care practitioner empathy and risk of cardiovascular events and all-cause mortality among patients with type 2 diabetes: a population-based prospective cohort study. The Annals of Family Medicine, 17, 311-318.
DIKMEN, B. T., BAYRAKTAR, N. & YıLMAZ, Ü. D. 2022. A qualitative study of medical-surgical intensive care unit nurses’ experiences in caring for critical patients. Revista da Escola de Enfermagem da USP, 56.
HASSANKHANI, H., SOHEILI, A., DEHGANNEZHAD, J. & POWERS, K. 2022. Lack of empathy in interaction between patient/family and healthcare professionals in an Iranian emergency department: a focused ethnographic study. Nursing And Midwifery Journal, 20, 1-16.
KHADEMI, M., MOHAMMADI, E. & VANAKI, Z. 2019. On the violation of hospitalized patients’ rights: A qualitative study. Nurs Ethics, 26, 576-586.
LEVETT-JONES, T., CANT, R. & LAPKIN, S. 2019. A systematic review of the effectiveness of empathy education for undergraduate nursing students. Nurse education today75, 80-94.
LEVETT-JONES, T., LAPKIN, S., GOVIND, N., PICH, J., HOFFMAN, K., JEONG, S. Y., NORTON, C. A., NOBLE, D., MACLELLAN, L., ROBINSON-REILLY, M. & EVERSON, N. 2017. Measuring the impact of a ‘point of view’ disability simulation on nursing students’ empathy using the Comprehensive State Empathy Scale. Nurse education today, 59, 75-81.
NILSEN, P. 2015. Making sense of implementation theories, models and frameworks. Implementation Science, 10, 53.
STREKALOVA, Y. A., KRIEGER, J. L., NEIL, J., CAUGHLIN, J. P., KLEINHEKSEL, A. & KOTRANZA, A. 2017. I understand how you feel: The language of empathy in virtual clinical training. Journal of Language and Social Psychology, 36, 61-79.
WINTER, R., LEANAGE, N., ROBERTS, N., NORMAN, R. I. & HOWICK, J. 2022. Experiences of empathy training in healthcare: A systematic review of qualitative studies. Patient Education and Counseling.
Image credit: Photo by pure julia on Unsplash
Atefeh Galehdarifard
Student Research Committee, Lorestan University of Medical Sciences, Khorramabad, Iran
Mojgan Khademi
Social Determinants of Health Research Center, Lorestan University of Medical Sciences, Khorramabad, Iran
Mohammad Gholami
Social Determinants of Health Research Center, Lorestan University of Medical Sciences, Khorramabad, Iran
Moloud Radfar
Department of psychiatric nursing, School of Nursing and Midwifery, Urmia University of Medical Sciences, Urmia, Iran
Farzad Ebrahimzadeh
Nutritional Health Research Center, Lorestan University of Medical Sciences, Khorramabad, Iran
Mohammad-Hasan Imani-Nasab
Social Determinants of Health Research Center, Lorestan University of Medical Sciences, Khorramabad, Iran
Read the original research in Evidence & Policy:
Galehdarifard, A. R. Moloud, Gholami, M. Khademi, M, Ebrahimzadeh, F. & Imani-Nasab, M-H. (2024). The impact of knowledge brokering on nurses’ empathy with patients receiving cardiac care: an experimental study. Evidence & Policy, DOI: 10.1332/17442648Y2024D000000035.
If you enjoyed this blog post, you may also be interested in reading:
How did UK policymaking in the COVID-19 response use science? Evidence from scientific advisers
Disclaimer: The views and opinions expressed on this blog site are solely those of the original blog post authors and other contributors. These views and opinions do not necessarily represent those of the Policy Press and/or any/all contributors to this site.